Development and evaluation of a “simulator-based” ultrasound training program for university teaching in obstetrics and gynecology–the prospective GynSim study
| Author | Johannes Weimer, Florian Recker, Annette Hasenburg, Holger Buggenhagen, Karla Karbach, Lia Beer, Andreas Weimer, Lina Schiestl, Liv Lorenz, Roman Kloeckner and Anna Dionysopoulou |
|---|
Objective
This study addresses the challenges of ultrasound education in obstetrics and gynecology, focusing on the potential benefits of simulation techniques in medical training. Aiming to evaluate the impact of a structured simulator-based training program, this prospective, randomized, interventional study examines its effects on educational outcomes for 5th year medical students.
Methods
A total of 153 medical students were randomized into two groups: one receiving both theoretical instruction and hands-on ultrasound simulator training (study group), and the other receiving only theoretical instruction (control group). The study assessed theoretical knowledge and practical skills at two time points: upon enrollment and at the end of the course. The practical skills were specifically evaluated using a dedicated test on the ultrasound simulator.
Selection of simulators
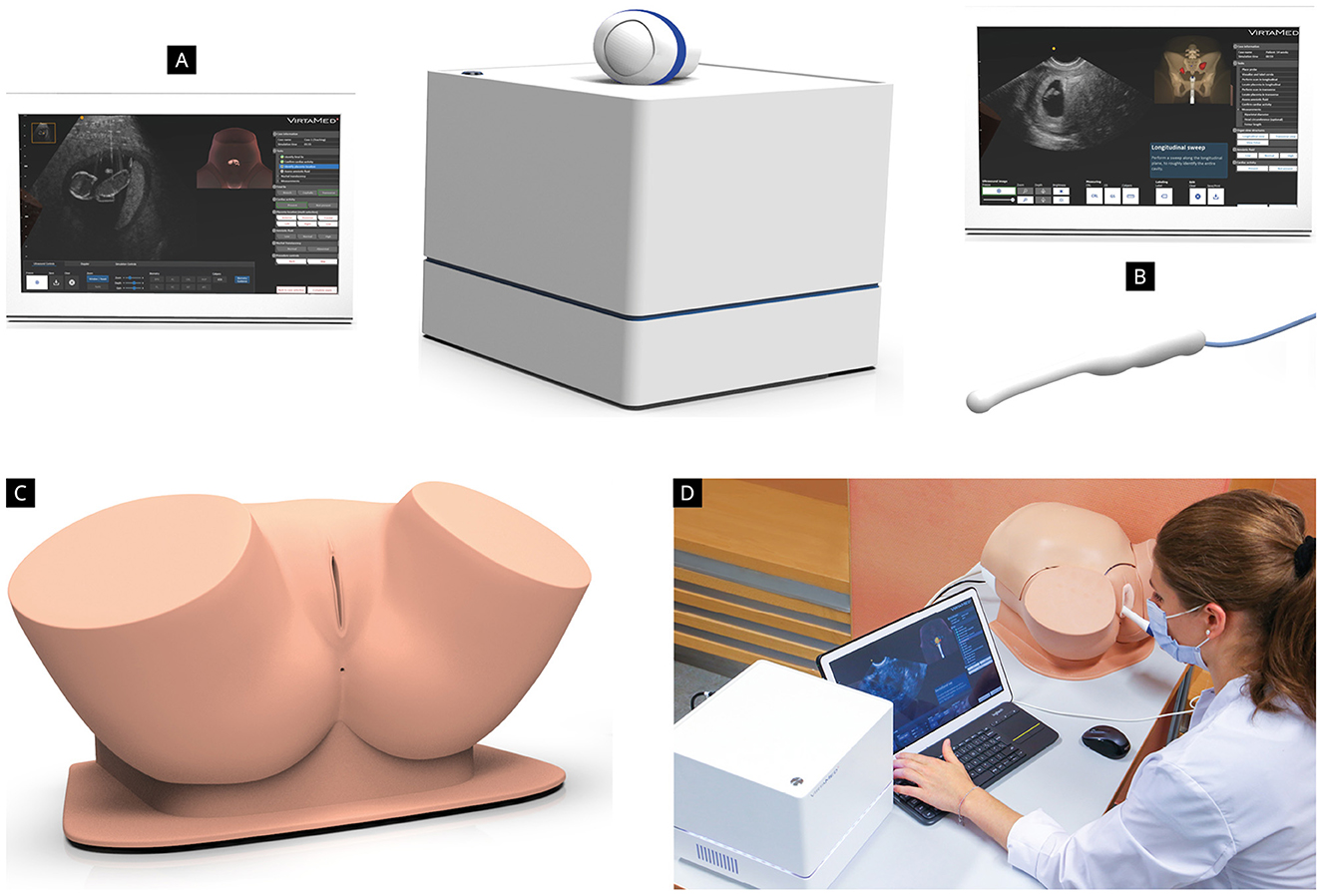
Prior to the study, we conducted a testing phase to determine which ultrasound simulator would best meet the needs of our study population. Therefore, we invited several ultrasound simulator companies to allow our medical team to test and evaluate their products. Three of them responded and agreed to take part to the this testing phase (Scantrainer 8:TAS/TVS OBGYN-Education pack), Skillsmed (Nuremberg, Germany), VirtaMed Portable GynoSTM OB/GYN ultrasound simulator (Zurich, Switzerland) and VIM-003 (Ob/Gyn) Simulator Base Unit, CAE Vimedix (Sarasota, United States). The three ultrasound simulators were installed in the Department of Obstetrics and Gynecology of the University Medical Center of the Johannes Gutenberg University Mainz and were available for testing for five working days. Twentysix participants (14 medical students, nine residents, and three consultants in Obstetrics and Gynecology) took part in this testing phase. The technical characteristics and functions of the simulators, the training platform and courses included in the software, as well as aspects like self-learning and simulator feedback were evaluated. We decided to conduct our study using the Virtamed Portable GynoSTM OB/GYN ultrasound simulator, since our colleagues’ evaluation showed a superiority of this simulator with regard to the above-mentioned aspects (Figure 2). The simulator includes transabdominal and transvaginal obstetric ultrasound modules with more than 100 cases available in the training platform.
Results
Out of 153 students, 113 completed the study (study group n=59, control group n=54). The students in the study group demonstrated a greater improvement in theoretical test scores. They also achieved better results at the practical test, with regard to image quality, accuracy, and efficiency. Both groups showed an increase in self-confidence and competency in performing ultrasound examinations independently. Students expressed high satisfaction with the course and a positive attitude toward simulator-based training.
Conclusion
The “GynSim” study marks a significant step forward in medical education for obstetrics and gynecology ultrasound training. This study shows how structured simulator-based training positively affects 5th-year medical students’ educational outcomes, enhancing their theoretical knowledge, practical skills, and confidence. The findings support the effectiveness of simulationbased training, noted for its methodological strength, including randomization, a large sample size, consistent teaching, and objective evaluation. These aspects ensure the study’s reliability and contribute insights into the benefits of simulator-based training, highlighting its role in preparing students for clinical practice and advocating for further research on its long-term benefits and curriculum integration to improve patient care and safety.